Tanya Andrews Physiotherapy
Shoulder
Acute Painful Shoulder
Not infrequently people will wake up with an acutely painful shoulder for no particular reason at all: they hadn’t overdone it in the gym, they hadn’t fallen down stairs or painted all the ceilings. And yet there they are with an incredibly painful shoulder that they can barely move. Normal painkillers don’t touch it and it just won’t go away. Quite a lot of people actually end up in A&E because the pain is so overwhelming. And mothers will often say the pain is worse than having children.
There are only two conditions that cause a severe, acute, painful shoulder coming on out of the blue and these are Calcifying Tendonitis and Brachial Neuritis: a simple x-ray will tell me which it is and how to treat it.
Calcifying Tendonitis
Calcifying tendonitis is where the main tendon that lifts the arm up in the air has been rubbing (or impinging) away quietly, possibly for years, without you knowing anything about it. In simple terms, the tendon bleeds a little and the body changes the blood slowly into chalk. It’s more like toothpaste consistency than blackboard chalk and it can sit in the tendon for years without causing any issues. Until suddenly it causes acute pain.
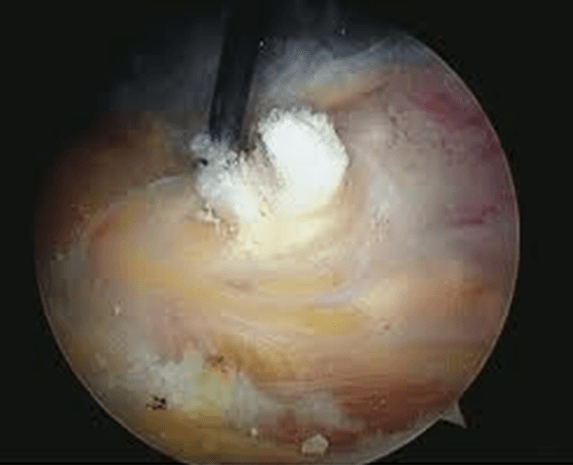
The dense white cloud is the chalk deposit in the tendon
What then happens is the chalk starts to be squeezed or extruded out of the tendon ( supraspinatus tendon) into the sub-acromial space and sets off the horrific inflammatory reaction causing the severe pain that means you simply don’t dare move your arm/shoulder.
But it is very treatable and a simple steroid and local anaesthetic injection into the sub-acromial space can get rid of it very quickly. That may not eliminate the pain completely but it is usually much, much better within a few hours and certainly manageable. Usually though you will need surgery a few weeks later to get rid of the residual discomfort and you may need an arthroscopic subacromial decompression which comprises of shaving away a little bit of bone to make more space for the tendons to glide freely in.
This is the chalk being removed arthroscopically
Neuralgic Amyotrophy
If the x-ray doesn’t show any chalk deposits then you have a condition called Brachial Neuritis or Parsonage Turner Syndrome or Neuralgic Amyotrophy. These are all terms that cover the same condition in which a virus inflames the nerves and muscles around the shoulder causing pain, pain, pain. There really isn’t anything that can be done for this condition other than managing the symptoms until it sorts itself out. You may be advised to see a Pain Management Specialist as they have the skills to organise an excellent regime of medication that can help control the pain without making you sleepy.
This acute and severely painful condition is NOT a frozen shoulder – they just don’t come on like this. It is the pain that means that you can’t move the shoulder not a freeze such as in Frozen shoulder.
Extracted partially from Mr Richard Sinnerton
Frozen Shoulder/Adhesive Capsulitis
A very common condition which is often misdiagnosed occurs in 2-5% of the population aged between 40-60 and more commonly women.
What is it?
It is not just a painful shoulder and it also is not just a shoulder that you can not move. It is defined as a global loss of passive movement with normal X Rays.
This means that not only can you not move it but nor can your doctor. The Xray is of vital importance to the correct diagnosis. This is because the other common cause of pain and stiffness in the shoulder is arthritis.
What happens to the joint in Frozen Shoulder?
The shoulder joint is a ball and socket joint surrounded by layers of skin,fat, muscles, ligaments and tendons that all hold it together and move it around. Those are all normal in a Frozen shoulder but what is not normal is the joint capsule. Normally this is thin and stretchy like Lycra but in a Frozen shoulder something upsets it causing it to thicken and lose its elasticity which in turn causes pain and loss of movement.
Causes
The trigger is not always clear and may not be result from anything dramatic you have done. Sometimes the trigger is more obvious such as after surgery on the shoulder,arm or chest or after a fall. People with diabetes and thyroid problems have a slightly higher risk.
A thorough and careful assessment is important because frozen shoulder is commonly misdiagnosed as being a rotator cuff tear. And people who have rotator cuff tears often are told they have frozen shoulder. Accordingly, it is critical that patients who are thought to have either condition be evaluated for the other to ensure an accurate diagnosis and proper treatment.
Diagnosis
The early stages of Frozen shoulder can be hard to diagnose as many of the symptoms are identical to tendonitis, which means painful on movement but it still moves reasonably well. The overriding symptom is pain.
This is called Stage 1 or the Freezing stage.
About 75% of people who are told they do not have a frozen shoulder do in fact have it.
By the time you consult your GP or a consultant the condition may have progressed to the Frozen stage.
The Frozen stage is when the shoulder will simply not move. You can test this by lying down on the floor and stretch both arms up over your head. The non affected arm will be able to touch the floor whereas the affected arm will be some way away.
Another test is you tuck your elbows in to your side and keeping them there with elbow bent to 90 degrees rotate the hand out away from the body. You will see a big difference in the range.
Thawing is the final stage where the capsule slowly recovers and the functional movement returns.
How long will it take?
If the shoulder isn’t too painful and isn’t stopping you doing the things you want to do or interfering with your sleep then you could chose to live with it. Wait it out patiently and it will get better. Eventually! If they are left alone most Frozen shoulders get better on their own but can take up to 18 months.
Treatment
If it is very painful in either the early stages or, very occasionally, the Frozen phases then the gleno-humeral joint injection is worth a go. This could leave you with a pain-free but stiff shoulder and you may be happy with that. It may also change the progression of the condition and start a rapid defrost and that would be an excellent result.
If however the restriction in movement has put your life on hold and you are struggling to work, to play with your children, participate in sports or to sleep then a manipulation under anaesthetic (MUA) could be the better choice for you.
The best time to do the MUA is when the shoulder has fully frozen up and not before. If you are operated during the freezing phase then the risk of re-freezing is higher. It may start off well after the surgery and then freezes up again. So that is why injections are suggested in the early phase.
In cases with significant pain and stiffness, an injection of a corticosteroid medication into the joint often is recommended. The injection into the joint is a very different sort of injection to the one either a GP might give you or that might be given for tendonitis. It is a steroid injection but it goes right into the gleno-humeral joint (ball and socket joint) where all the freezing activity is actually taking place. It is usually done by a radiologist ( a Consultant specialising in imaging) in the X-ray department and they use either the Ultra-sound scanner or an Image Intensifier (a moving x-ray machine) to guide the needle into the right place. For NHS patients it may be offered as a day-case in the operating theatre with you lightly sedated.
However, once the shoulder is fully frozen then they don’t have any effect.
Stiffness that lasts beyond a full course of physiotherapy over six to 12 months or shoulder stiffness that gets significantly worse during physiotherapy may signal that the surgery is needed to release the tight ligaments and remove scar tissue that may contribute to the problem. The surgery usually can be done arthroscopically through two to three small incisions as an outpatient procedure, so an overnight hospital stay is not required. Physiotherapy is still necessary for several weeks or more after surgery to prevent frozen shoulder from coming back.
After it’s been successfully treated, it’s uncommon for frozen shoulder to return in the same shoulder. But some patients may go on to have it in the other shoulder. In people who have medical issues that put them at risk for the condition, treating the underlying disorder may decrease the likelihood of developing frozen shoulder.
What can I do myself to help the pain?
Self help is normally the best form of treatment - full recovery for this condition may take a long time. The aim of treatment is to ease pain and stiffness and keep the movement of the shoulder as good as possible whilst encouraging the condition to clear.
- Medication - Anti-inflammatory tablets or painkillers may have been prescribed or alternatively can be purchased from a pharmacy. These may help with stiffness and pain but may not be suitable for all patients. Paracetamol maybe a suitable alternative. If in doubt you should consult your GP or pharmacist before taking any medication.
- Heat - May be useful. Use a wheat bag or hot water bottle wrapped in a towel for 15 minutes as often as required. Ensure the pack is not too hot to avoid burning the skin.
- Ice - some people find ice more helpful than heat. Apply a cold pack for 15 minutes to the affected shoulder. You may repeat every 3-4 hours. Do not apply the ice directly to the skin (place a damp cloth between your skin and the ice to avoid ice burns).
- Pillows - Adopt a comfortable position. Lying on the unaffected side with a pillow under the affected arm can be comfortable.You may also place a pillow behind you whilst on your side to prevent you from rolling over.
- Exercise —Gentle exercise is advised to maintain available range of movement during all 3 stages of the condition and encourage a successful recovery of any lost movement as the condition resolves.
Exercises/ Physiotherapy
Exercise is advised to maintain available movement during all 3 stages. Initially these should only be performed within the boundary of pain. There may be some level of discomfort while exercising. If discomfort increases after completion of the exercises then reduce the number of repetitions of the exercises but do not stop altogether.
If you have associated pain from the neck and back the physiotherapist will also be able to help you with this.
A physiotherapist will come in to their own once you reach stage 3 or after surgery. They can provide exercises to help restore the shoulder’s range of motion and mobility. They will help stretch all the tight structures and give you a graduated exercise program for you to perform at home. They will be paramount in restoring the shoulder back to full strength and mobility.
Some examples of early exercises are below:
- Stand leaning forwards fully supported with the unaffected hand.Let the affected arm hang down, let it relax. Gently swing your arm backwards and forwards,side to side, and in circles.Repeat each direction up to 10 times.Do 2 –3 times a day.
- Lying on your back, support your affected arm with your non affected arm with your elbows straight. Use one arm to lift the other over your head, keeping it as close to the ear as possible.Repeat up to 10 times.Do 2 –3 times a day.
- Stand with your elbows bent to 90◦ holding a stick in front of you. Gently push the stick sideways across your body.Keep your elbow tucked into your side, feel the stretch in the shoulder. Hold for 20 – 30 seconds. Repeat 5 times, 2-3 times per day.
The following exercises may be helpful in stage 3 as the condition improves.
- Stand or sit. Stretch one arm over the opposite shoulder by pushing it at the wrist with your other arm. Hold the stretch for approx 20 - 30 seconds then relax. Repeat 5 times, 2-3 times per day.
- Stand or sit. With one arm bring a towel over your shoulder behind your back. Hold the towel as shown.Gently pull upwards stretching the affected arm behind your back.Hold for approx 20 - 30 seconds.Repeat 5 times, 2-3 times per day.